Treating Telangiectatic Matting

Cutaneous necrosis is relatively rare and often of limited sequelae but most commonly related to extravasation of sclerosant.
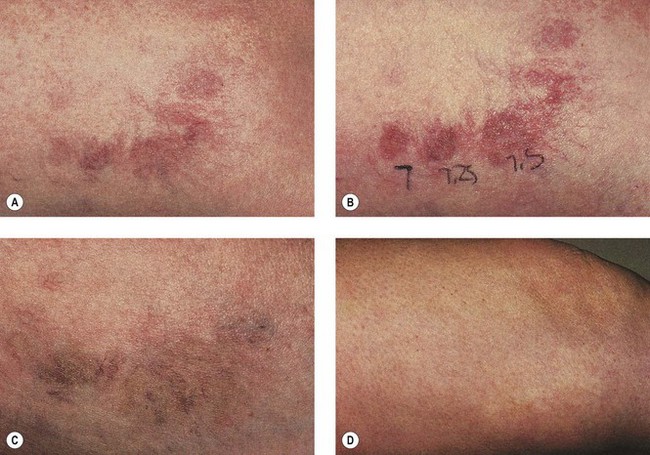
Treating telangiectatic matting. Systemic anticoagulant agents and systemic steroids may be used when extensive necrosis is anticipated. If reflux is present consider medical treatment as well. Work outdoors sit or stand all day misuse alcohol are pregnant are older or elderly telangiectases are more likely to form as skin ages have rosacea scleroderma dermatomyositis or systemic lupus erythematosus sle use corticosteroids. Telangiectatic matting and hyperpigmentation are some of the most commonly observed side effects of sclerotherapy.
A study comparing different times of postsclerotherapy compression in treating leg telangiectasia also demonstrated a decrease in tm when compression was maintained for one to three weeks 5 versus three days 30 or no compression 40 21 this is most likely a reflection of a decrease in intravascular thrombosis with prolonged graduated compression which results in a decreased phlebitic effect with decreased inflammation. If this happens it can also be treated with another sclerotherapy session for more adequate temporary cosmetic results. This includes those who. Before your vein doctor gives you additional sclerotherapy varicose vein treatment he or she will need to look for the root cause of the telangiectatic matting.
Intense pulsed light therapy ipl is also sometimes used to eliminate telangiectatic matting.